Frequently Asked Questions About Melanoma
What Is Melanoma?
Melanoma skin cancer accounts for only 1% of all skin cancers, but it is more likely to grow and spread. As a result, melanoma is responsible for a large majority of skin cancer deaths, making early detection and treatment very important.
Melanoma is a cancer that arises from a type of skin cell known as a melanocyte. Melanocytes produce a brown pigment called melanin, which protects the deeper layers of the skin from some of the harmful effects of the sun. When skin is exposed to sunlight, melanocytes produce more melanin, causing the skin to tan or darken.
Generally, melanoma cells continue to produce melanin, so melanoma skin cancers are typically brown or black. However, some melanomas can appear tan, pink or even white because they do not produce melanin.
Dark brown or black skin is not a guarantee against melanoma. African Americans can develop this cancer, especially on the palms of the hands, soles of the feet, under nails, or in the mouth.
What are the risk factors for melanoma?
- Exposure to ultraviolet light. Sunlight is the primary source of ultraviolet (UV) rays, which damage the DNA of skin cells. Other sources of UV rays include tanning beds and sun lamps.
- Moles. A mole is a noncancerous pigmented tumor. Most moles never turn into cancer, but people with many moles are more likely to develop melanoma. Atypical moles—moles that are larger than normal or have an abnormal shape or color—are called dysplastic nevi. Dysplastic nevi often run in families. Dysplastic nevus syndrome, also known as familial atypical multiple mole melanoma syndrome (FAMMM), is an inherited condition associated with many dysplastic nevi and at least one close relative who has had melanoma. People with dysplastic nevus syndrome have a very high lifetime risk of melanoma. Congenital melanocytic nevi are moles that are present at birth. Lifetime risk of melanoma developing in a congenital melanocytic nevus is estimated to be 0-10%, and risk increases as the size of the mole increases.
- Fair skin, light hair and freckles. Melanoma is more common in people with fair complexions.
- Family history of melanoma. Risk is higher in people who have one or more first-degree relatives with melanoma.
- Personal history of melanoma or other skin cancers. People who have had melanoma are at higher risk of getting melanoma again.
- Age. While melanoma is more likely to occur in older people, it is also one of the most common cancer in people under age 30.
- Having a weakened immune system. People with weakened immune systems (from certain diseases or medical treatments) are more likely to develop melanoma and other skin cancers.
- Xeroderma pigmentosum. This rare inherited condition affects the ability of skin cells to repair damage to their DNA.
Where is melanoma most often found?
Melanoma most often appears on fair-skinned men and women, but people with other skin types can be affected. In men, melanoma most often appears on the chest or back. In women, the arms and legs are more common sites. It can also develop on the face, neck, or other areas. Rarely, melanomas can form in parts of the body not covered by skin, such as the eyes, mouth, vagina, large intestine, and other internal organs.
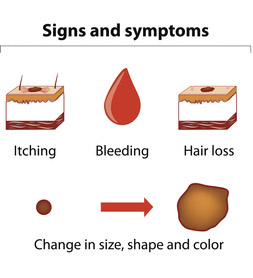
What are the signs and symptoms of melanoma?
Common signs of melanoma are asymmetry or irregularity, changes in color or color variations in a mole, a spot larger than the size of pencil eraser, or a spot that is evolving and changing in size, shape or color. Oozing or bleeding from a mole, a mole that looks different from your other moles or feels itchy, hard, lumpy, swollen, or tender to the touch, can also be signs of a malignant melanoma.
Because most malignant melanoma cells still produce melanin, melanoma tumors are often shaded brown or black. Melanoma can also appear on the body as a new mole. Melanoma can spread quickly to other parts of the body through the lymph system, or through the blood. Like most cancers, melanoma is best treated when it is diagnosed early. The symptoms of melanoma may resemble other conditions or medical problems. Always consult your doctor for a diagnosis.
What does melanoma look like?
Visit Skin Cancer Symptoms for more information and for pictures of melanoma.
What is melanoma staging?
Once a melanoma has been diagnosed, a process called staging provides important information about the extent of the skin cancer and its anticipated response to treatment. Your physician will assign a stage according to the degree of severity of the cancer. Melanoma staging is also useful for estimating prognosis.
Generally, lower stage cancers have a better outlook for cure or long-term survival, but other factors may also affect prognosis. The stages of melanoma run from stage 0, the earliest possible stage, in which the melanoma is confined to the top layers of the skin – also known as melanoma in situ – to stage 4 melanoma, in which the cancer has spread beyond the original area of the skin and nearby lymph nodes to other organs, distant areas of the skin or distant lymph nodes.



