Understanding Brain Aneurysms
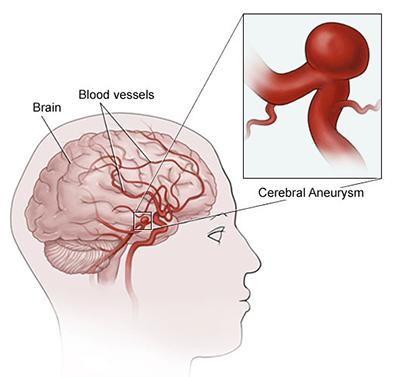
A brain aneurysm (also called an cerebral aneurysm or intracranial aneurysm) is a bulging, weakened area in the wall of an artery in the brain, resulting in an abnormal widening, ballooning, or bleb. Because there is a weakened spot in the aneurysm wall, there is a risk for rupture (bursting) of the aneurysm.
A brain aneurysm more frequently occurs in an artery located in the front part of the brain that supplies oxygen-rich blood to the brain tissue. Arteries anywhere in the brain can develop aneurysms. A normal artery wall is made up of three layers. The aneurysm wall is thin and weak because of an abnormal loss or absence of the muscular layer of the artery wall, leaving only two layers.
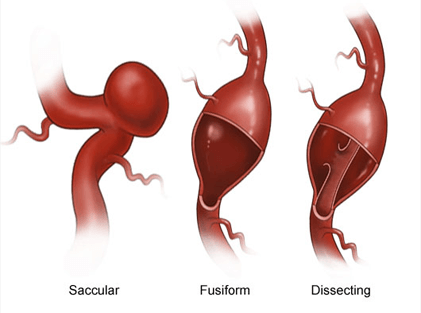
The most common type of brain aneurysm is called a saccular, or berry, aneurysm, occurring in 90 percent of brain aneurysms. This type of aneurysm looks like a "berry" with a narrow stem. More than one aneurysm may be present.
Two other types of brain aneurysms are fusiform and dissecting aneurysms.
- A fusiform aneurysm bulges out on all sides (circumferentially), forming a dilated artery. Fusiform aneurysms are often associated with atherosclerosis.
- A dissecting aneurysm results from a tear along the length of the artery in the inner layer of the artery wall, causing blood to leak in between the layers of the wall. This may cause a ballooning out on one side of the artery wall, or it may block off or obstruct blood flow through the artery. Dissecting aneurysms usually occur from traumatic injury, but they can also happen spontaneously. The shape and location of the aneurysm may determine which treatment is recommended.
Most brain aneurysms (90%) present without any symptoms and are small in size (less than 10 millimeters, or less than four-tenths of an inch, in diameter). Smaller aneurysms may have a lower risk of rupture.
Although a brain aneurysm may be present without symptoms, the most common initial symptom of a cerebral saccular aneurysm is a sudden headache from a subarachnoid hemorrhage (SAH). SAH is bleeding into the subarachnoid space (the space between the brain and the membranes that cover the brain) and not into the brain tissue. Minor subarachnoid hemorrhage most frequently occurs following head trauma. Major subarachnoid hemorrhage is most commonly from a ruptured cerebral saccular aneurysm (80 percent). A sudden headache associated with SAH is a medical emergency.
Increased risk for aneurysm rupture is associated with aneurysms that are over 10 millimeters (less than four-tenths of an inch) in diameter, a location (circulation in the back portion of the brain), and/or previous rupture of another aneurysm. A significant risk of death is associated with the rupture of a brain aneurysm.
What Causes a Brain Aneurysm?
Currently, the cause of brain aneurysms is not clearly understood. Brain aneurysms are associated with several factors, including smoking, hypertension, and family history (genetic). The ultimate cause of a brain aneurysm is an abnormal degenerative (breaking down) change (weakening) in the wall of an artery, and the effects of pressure from the pulsations of blood being pumped forward through the arteries in the brain. Certain locations of an aneurysm may create greater pressure on the aneurysm, such as at a bifurcation.
Inherited risk factors associated with aneurysm formation may include the following:
- Alpha-glucosidase deficiency. A complete or partial deficiency of the lysosomal enzyme, alpha-glucosidase. This enzyme is necessary to break down glycogen and to convert it into glucose.
- Alpha 1-antitrypsin deficiency. A hereditary disease that may lead to hepatitis and cirrhosis of the liver or emphysema of the lungs.
- Arteriovenous malformation, or AVM. An abnormal connection between an artery and a vein.
- Coarctation of the aorta. A narrowing of the aorta, the main artery coming from the heart.
- Ehlers-Danlos syndrome. A connective tissue disorder (less common).
- Family history of aneurysms
- Female gender
- Fibromuscular dysplasia. An arterial disease, cause unknown, that most often affects the medium and large arteries of young to middle-aged women.
- Hereditary hemorrhagic telangiectasia. A genetic disorder of the blood vessels in which there is a tendency to form blood vessels that lack capillaries between an artery and vein.
- Klinefelter syndrome. A genetic condition in men in which an extra X sex chromosome is present.
- Noonan's syndrome. A genetic disorder that causes abnormal development of many parts and systems of the body.
- Polycystic kidney disease (PCKD). A genetic disorder characterized by the growth of numerous cysts filled with fluid in the kidneys. PCKD is the most common medical disease associated with saccular aneurysms.
- Tuberous sclerosis. A type of neurocutaneous syndrome that can cause tumors to grow inside the brain, spinal cord, organs, skin, and skeletal bones.
Acquired risk factors associated with aneurysm formation may include the following:
- Advancing age
- Alcohol consumption (especially binge drinking)
- Atherosclerosis. A buildup of plaque (made up of deposits of fatty substances, cholesterol, cellular waste products, calcium, and fibrin) in the inner lining of an artery.
- Cigarette smoking
- Use of illicit drugs such as cocaine or amphetamine
- Hypertension (high blood pressure)
- Trauma (injury) to the head
- Infection
A risk factor is anything that may increase a person's chance of developing a disease. It may be an activity, such as smoking, diet, family history, or many other things. Different diseases have different risk factors.
Although these risk factors increase a person's risk, they do not necessarily cause the disease. Some people with one or more risk factors never develop the disease, while others develop disease and have no known risk factors. Knowing your risk factors to any disease can help to guide you into the appropriate actions, including changing behaviors and being clinically monitored for the disease.
Symptoms of a Brain Aneurysm
Seek medical attention immediately if you are experiencing some or all of the symptoms listed under warning signs/symptoms. The presence of a brain aneurysm may not be known until the time of rupture. However, occasionally there may be symptoms that occur prior to an actual rupture due to a small amount of blood that may leak, called "sentinel hemorrhage" into the brain. Some aneurysms are symptomatic because they press on adjacent structures, such as nerves to the eye. They can cause visual loss or diminished eye movements, even if the aneurysm has not ruptured.
The symptoms of an unruptured brain aneurysm include, but are not limited to, the following:
- Headaches (rare, if unruptured)
- Eye pain
- Vision deficits (problems with seeing)
- Eye movement deficits
The first evidence of a brain aneurysm is most frequently a subarachnoid hemorrhage (SAH), due to rupture of the aneurysm. Symptoms that may occur at the time of SAH include the following:
- Initial sign (rapid onset of "worst headache of my life")
- Stiff neck
- Nausea and vomiting
- Changes in mental status, such as drowsiness
- Pain in specific areas, such as the eyes
- Dilated pupils
- Loss of consciousness
- Hypertension (high blood pressure)
- Motor deficits (loss of balance or coordination)
- Photophobia (sensitivity to light)
- Back or leg pain
- Cranial nerve deficits (problems with certain functions of the eyes, nose, tongue, and/or ears that are controlled by one or more of the 12 cranial nerves)
- Coma and death
The symptoms of a brain aneurysm may resemble other problems or medical conditions. Always consult your doctor for a diagnosis.
How Is a Brain Aneurysm Diagnosed?
A brain aneurysm is often discovered after it has ruptured or by chance during diagnostic examinations such as computed tomography (CT scan), magnetic resonance imaging (MRI), or CT angiography that are being done for other reasons. In addition to a complete medical history and physical examination, diagnostic procedures for a brain aneurysm may include the following:
- Diagnostic cerebral angiogram/digital subtraction angiography (DSA). Provides an image of the blood vessels in the brain to detect a problem with vessels and blood flow. The procedure involves inserting a catheter (a small, thin tube) into an artery in the leg and passing it up to the blood vessels in the brain. Contrast dye is injected through the catheter and X-ray images are taken of the blood vessels.
- Computed tomography scan (CT or CAT scan). A diagnostic imaging procedure that uses a combination of X-rays and computer technology to produce cross-sectional horizontal, or axial, images (often called slices) of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general X-rays, and may be used to detect abnormalities and help identify the location or type of stroke. A CT angiogram (CTA) can also be obtained on a CT scan to look at the vessels.
- Magnetic resonance imaging (MRI). A diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body. An MRI uses magnetic fields to detect small changes in brain tissue that help to locate and diagnose a stroke.
- Magnetic resonance angiography (MRA). A noninvasive diagnostic procedure that uses a combination of magnetic resonance technology (MRI) and intravenous (IV) contrast dye to visualize blood vessels. Contrast dye causes blood vessels to appear opaque on the MRI image, allowing the doctor to visualize the blood vessels being evaluated.
Click here to request more info about the Brain Aneurysm Program online or call us at 1-888-724-7123.



