Pancreaticobiliary Endoscopy
Endoscopic Ultrasonography (EUS) with fine needle aspiration
Endoscopic Ultrasound with Fine Needle Aspiration is a minimally invasive procedure that can be used to obtain tissue samples from lesions around the gastrointestinal tract to aid in diagnosis. It involves advancing a special endoscope into the stomach or small intestine, and using ultrasound from inside the gastrointestinal lumen to visualize the deep layers of the gastrointestinal walls as well as structures nearby to the lumen including the pancreas, the liver, and lymph nodes. Once visualized, a needle can be advanced from the scope into the desired lesion under direct visualization to obtain cells to be examined under a microscope.

Endoscopic Retrograde Cholangiopancreatography (ERCP)
Endoscopic Retrograde Cholangiopancreatography (ERCP) is a procedure that allows for alleviation of obstruction of the ducts that drain the liver/gallbladder and pancreas.
During ERCP, access is obtained into either the bile duct or the pancreatic
duct and the opening is enlarged using a technique called a sphincterotomy.
A balloon is used to inflate high-up in the duct to sweep out stones causing
an obstruction. In some cases where a stricture is present (a narrowing
of the duct either from inflammation or cancer), a stent is placed which
stretches the narrowed area open over time and allows for continued drainage
even after the procedure concludes. Biopsies of the bile duct or pancreatic
duct may also be obtained when necessary.
Some stones in the bile duct or pancreatic duct are too large to be swept
out with a balloon. In these cases, there are several novel techniques
to facilitate removal. There are special baskets that can be used to surround
a stone and crush it into small pieces which can then be removed. Additionally,
a special laser can be advanced into the bile duct or pancreatic duct
to blast a large stone into small pieces so that it can be removed. This
is called laser lithotripsy.
ERCP is also performed when there is a leak in the bile duct or pancreatic
duct, meaning a hole in the duct that allows toxic bilious or pancreatic
fluid to leak into the surrounding abdomen. By placing a stent across
the leak, it can be sealed, allowing it to heal over time.
- Gallstones (most common)
- Ampullary adenoma / Ampullary cancer
- Primary sclerosing cholangitis
- Autoimmune pancreatitis
- Metastatic cancer invading the bile duct
- Pancreatic cancer
- Primary bile duct cancer (cholangiocarcinoma)
- Acute pancreatitis
- Chronic pancreatitis
Biliary Ablation Therapies
-
Photodynamic Therapy (PDT)
Primary bile duct cancer, also called cholangiocarcinoma, is a cancer with poor survival rates. Surgery is the only cure, and advanced disease limits the option to undergo surgery at the time of diagnosis. PDT is a technology that can be used in conjunction with chemotherapy to prolong survival. This technique involves receiving an infusion of a light-activated medication that is absorbed by bile duct cancer cells. Forty-eight hours later, light is applied to the bile duct during ERCP causing the cancer cells to die. Studies have shown this technology to be safe and to increase survival in patients with cholangiocarcinoma. -
Biliary Radiofrequency Ablation (RFA)
In patients with bile duct obstruction from any type of cancer, RFA to the bile duct during ERCP can be used in conjunction with chemotherapy to prolong survival. This technique works by applying thermal energy to the bile duct tissue which results in coagulation necrosis and death of cancer cells. In studies, it has been shown to improve how long the narrowing in the bile duct remains open, decreasing the need for repeat procedures to exchange stents. In addition, it is associated with a survival benefit.
Extra Corporeal Shock Wave Lithotripsy (ESWL)
Some patients with pancreatitis have very large and hard stones that cannot be blasted with the special laser during ERCP. For these patients, a unique technology is offered, called extra corporeal shock wave lithotripsy. This technology directs shock waves from outside the body directly at the stone, causing it to break into pieces which can then be subsequently removed during endoscopy.
Advanced Pancreaticobiliary Imaging
Sometimes, it can be difficult to know if a stricture (narrowing) in the bile duct or pancreatic duct is due to cancer or to inflammation. Biopsies can be helpful, but sometimes they can be negative even in the setting of cancer. Therefore, a variety of imaging techniques are available to aid in making the correct diagnosis.
-
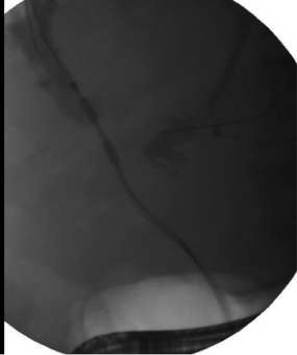
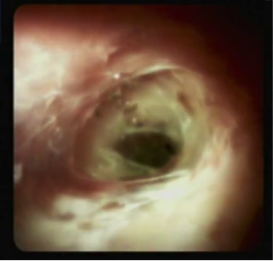
SpyGlass® Digital Cholangiopancreatoscopy
During ERCP, the bile duct is visualized using X-rays – contrast is injected into the bile duct which shows up on X-ray, and pathology is diagnosed by areas that don’t fill or are narrowed. Cholangiopancreatoscopy is a novel and exciting technology that allows a small camera to be inserted into the bile duct or pancreatic duct so that the inside of the duct can be examined visually. In addition, biopsies can be targeted to areas that look especially suspicious, increasing the chance of making an accurate diagnosis.
-
Optical coherence tomography (VLE)
OCT is the newest pancreaticobiliary imaging tool. This device uses infrared light to obtain high-resolution, cross-sectional imaging of tissue microstructure below the surface that can be interpreted in real-time. Although new, preliminary studies have shown that certain findings on OCT are highly predictive of having a cancer diagnosis.

