Knowing the signs and acting fast can make all the difference.
Do you know the signs of a stroke? Recognizing them could save a life—perhaps your own—and minimize a stroke’s potential life-changing effects.
“Unfortunately, people with stroke symptoms often put off calling for an ambulance because they think the symptom will pass or doesn’t signify a more significant health issue,” says Karen Vargas, RN, MSN, Stroke Program Coordinator for Robert Wood Johnson University Hospital (RWJUH) Rahway.
“When someone notices a friend or family member not acting like themselves, they should call an ambulance and also make note of the time,” she says. “The sooner a doctor sees a patient, the sooner they can determine whether the underlying cause of the symptom is a stroke—and the more effective treatment is likely to be.”
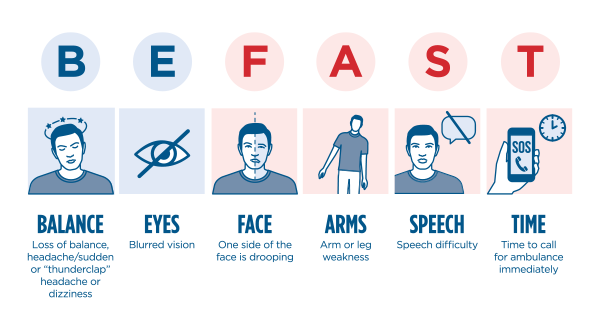
The memory trick known as “B.E. F.A.S.T.” makes it easier for people to better connect suspicious symptoms with the possibility that a stroke is causing the issue. Warning signs include:
B for Balance: Dizziness, a fall, or vertigo.
E for Eyes: Blurred vision or loss of vision.
F for Face: A slight droop, an uneven smile or a change in the way the eyes look.
A for Arm: Is one arm weak or does it feel heavy and difficult to lift?
S for Speech: Is there slurred speech or an inability to get words out?
T for Time: Time to call 911.
Don’t delay help for a potential stroke victim. Call 911 rather than calling a doctor or driving the ill person to the emergency department. Emergency responders can communicate effectively with the hospital and even begin treatment on the way there, Vargas explains.
A Team For Treatment
Once at the hospital, a stroke patient requires a team of specialists, including a physician, nurse, neurologist, radiologist, lab technicians and stroke coordinator, Vargas says.
“We work as a team to ensure that the hospital provides the highest level of care in the diagnosis and treatment of patients affected by strokes and other cerebrovascular diseases,” Vargas explains. She collects and analyzes the data associated with established clinical practice guidelines so she can collaborate with the team in the creation, implementation and evaluation of standards of care.
“Another important aspect of the role is educating the community about the signs and symptoms of stroke, as well as stroke prevention,” she explains. One of her most important duties is turning complicated scientific information into usable and easy-to-understand terms.
“The words I might use to explain what a stroke feels like are ‘Pay attention when you feel something different or something you’ve never felt before,’” Vargas says.
This awareness is especially important because many people suffer ministrokes before having a bigger one. “Your family might notice slurred speech or a facial difference, but you’re the best person to know that something’s not right,” she adds. “You know your own body.”
The Three Types of StrokesNo matter what type of stroke a person suffers, time is always of the essence when it comes to treatment.
|
Who's At Risk For a Stroke?Risk Factors You Can't Control:
Risk Factors You Can Control:
|
To educate your group, club or organization on the signs and symptoms of stroke, call RWJUH Rahway Community Education at 732-499-6193.