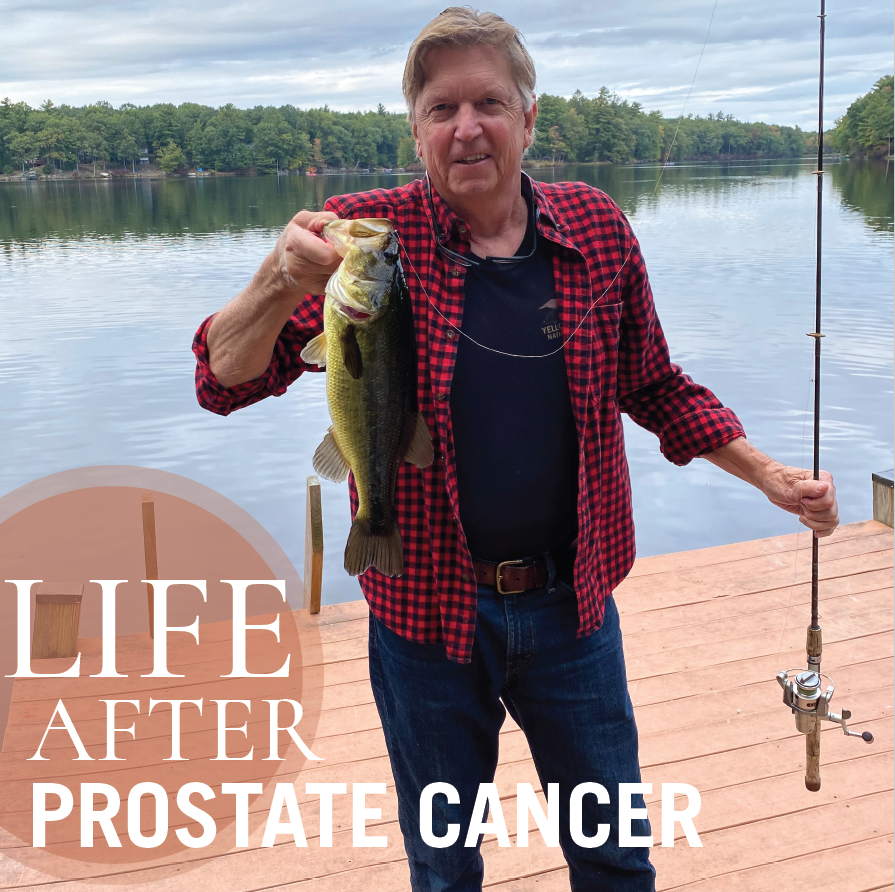
David Simpson, prostate cancer survivor, shows off his catch in the Delaware Highlands.
Advanced radiation therapy allows a local man to get back to his hobbies.
David Simpson, 68, takes an active retirement to a whole new level. On any given day, the Florham Park resident may be skiing, biking, hiking, fishing, golfing, kayaking or spending time with his wife, JoAnne, their two daughters and three grandchildren. “I’m a man with too many hobbies,” David says with a chuckle.
In early 2018, he added another hobby to his list: health detective.
Because his father had battled prostate cancer years earlier, David knew the benefit of regular screening. He’d asked his family doctor for yearly prostate-specific antigen (PSA) blood tests, which physicians use to find prostate cancer at its earliest stages. Though every individual is different, a PSA level under 4 is generally considered healthy.
“Over the years my PSA level went from 2 to 3 to 5,” David says. “Early in 2018, it was 6.4, so my family doctor asked me to see a urologist.” A biopsy revealed that David had prostate cancer.
“They gave me the choice to do nothing and wait to see if the PSA levels increased and the cancer spread, or to get it treated,” David says. “I said, ‘Why wait?’”
Looking at Options
Before deciding on a treatment option, David put on his detective hat. He scoured the internet for information and met with four different doctors. He also talked to friends, some of whom had battled prostate cancer with varying degrees of success.
“I investigated the pros and cons of every treatment out there,” he says. “I was worried about side effects like incontinence and sexual dysfunction and wanted the best chance of avoiding them.”
Eventually, he met with Alison Grann, MD, Chair of the Department of Radiation at Saint Barnabas Medical Center, who is also the Director of Network Integration and Quality, Radiation Oncology, Northern Region, at RWJBarnabas Health. Dr. Grann suggested a treatment called CyberKnife®.

Despite the word “knife,” CyberKnife doesn’t involve any cutting. Instead, it’s a form of stereotactic body radiation therapy, a very precise method that delivers radiation directly where it’s needed and spares healthy tissue. In David’s case, radiation would target the prostate while avoiding the bladder and rectum. Dr. Grann’s team also uses SpaceOAR Hydrogel, which temporarily positions the anterior rectal wall away from the prostate during radiation therapy, significantly reducing the rectum’s exposure.
CyberKnife is a small radiation machine located on top of a robot. During treatment, patients lie faceup on a table inside a radiation oncology suite while the robot rotates around the patient in any direction, taking images every 10 seconds to guide the proper delivery of radiation.
“The prostate’s position in the body causes it to move around a lot. Even a gas bubble can cause movement,” Dr. Grann explains. “CyberKnife allows us to track the motion of the prostate so we can ensure high doses of radiation get sent safely to just the prostate. And because CyberKnife moves around the patient, it can deliver radiation from different angles.”
While older methods of radiation therapy required nine weeks of treatment, most CyberKnife patients need only five treatments, each one lasting 25 to 40 minutes.
“Many studies had shown that higher and more accurate doses of radiation for shorter periods of time shorter periods of time were safer,” Dr. Grann says. “CyberKnife is an excellent technology to ensure that treatment is delivered safely.”
Dr. Grann has been using CyberKnife for five years with impressive results. “It’s a viable treatment option for people like David who have low-risk prostate cancer and want to continue their lives with minimal inconvenience,” she says.
Brief Treatment
Once David met Dr. Grann and learned about CyberKnife, he knew it was right for him. “Dr. Grann took me inside the ‘control room’—it looked like they were getting ready for a NASA space launch,” he says. “Dr. Grann was very personable, and the medical center is just 10 minutes from my house. It’s where my daughters were born. I liked everything about it.”
David’s CyberKnife treatments lasted just two-and-a-half weeks. While all prostate cancer treatments carry the risk of sexual dysfunction—and all radiation can bring side effects such as frequent urination or inflammation of the prostate gland—David had no side effects.
“I’d lie there for an hour during radiation, listen to my choice of music, then I’d drive home,” he says. “I’d be tired and a little sore, but that was all.”
A blood test three months after treatment revealed that David’s PSA level had gone down to 0.5. Now it’s at 0.3, a sign that his prostate cancer is in remission. “Dr. Grann says that once she sees a number of 1 or less, it won’t likely change,” he says.
Today, David has new hobbies and is more active than ever. And he has a message for other men with prostate cancer. “Don’t wait,” he says. “Get it taken care of.”
RWJBarnabas Health and the Cancer Center at Saint Barnabas Medical Center, together with Rutgers Cancer Institute of New Jersey—the state’s only NCI-Designated Comprehensive Cancer Center—provide close-to-home access to the latest treatment options. To learn more, call 844.CANCERNJ or visit the Cancer Center at Saint Barnabas Medical Center.
Learn more about CyberKnife at Saint Barnabas Medical Center.