“Miraculously, I regained all movement and speech”

With quick action, a multidisciplinary neurocritical care team identifies a hemorrhagic stroke in progress and prevents long-term effects.
In November 2019, David* and his wife, Ann*, were helping Ann’s mother clean out her home. David, a physician, was going through a drawer when, all of a sudden, he felt the urge to lie down. “I couldn’t talk, and I couldn’t move half of my body,” recalls David, 56.
Shortly afterward, Ann found him lying on the floor.
“I called 911,” says Ann, 55, who is also a physician. “I thought he might have bleeding in the brain, so I wanted him to go to a Comprehensive Stroke Center.”
An advanced life support ambulance picked up David and brought him to Robert Wood Johnson University Hospital (RWJUH). The paramedics had notified the hospital that a stroke patient was on the way, so the Code Stroke team was able to prepare for David’s arrival in the Emergency Department (ED).
Deviyani Mehta, MD, a stroke neurologist and Associate Professor of Neurology at Rutgers Robert Wood Johnson Medical School and RWJUH, was the attending physician on duty when David arrived. Ian Hakkinen, MD, a third-year neurology resident at Rutgers Robert Wood Johnson Medical School and RWJUH, spoke with Ann and was instrumental in ensuring quick treatment.

Reversing Stroke Damage
The team had to determine what kind of stroke David had suffered—a hemorrhagic stroke, which occurs when a weakened blood vessel in the brain bursts and starts bleeding, or an ischemic stroke, which is caused by a blood clot. A CT scan showed he didn’t have any bleeding in the brain. That finding, combined with the fact that he had arrived at the hospital within 4.5 hours of the onset of symptoms, made him a good candidate for tissue plasminogen activator (tPA), a clot-busting drug.
Next, he had a CT angiogram of the head and neck, in which a dye is injected into a vein and CT images of blood vessels are taken. The results revealed a blood clot in a large blood vessel on the left side of David’s brain, which controls the right side of the body.
Within 30 minutes of his arrival in the ED, David was given tPA. In some cases, that’s the only treatment a patient needs. In others, tPA is not sufficient to break apart a large clot blocking a blood vessel, and a patient requires a mechanical thrombectomy, in which a blood clot is removed from the brain. That was the case for David.
Fortunately, RWJUH is a Comprehensive Stroke Center, which means it provides the most advanced, multidisciplinary stroke care available. A Comprehensive Stroke Center must have stroke specialists, a unit dedicated to the care of stroke patients, a team of neurosurgeons and a Neurointensive Care Unit. Physicians are able to perform mechanical thrombectomies. If David had gone to another hospital, he might have required a transfer by helicopter to RWJUH or another Comprehensive Stroke Center.
After David received tPA, he was moved to the Neuro Intervention suite, where he underwent the thrombectomy, which was performed by Emad Nourollahzadeh, MD, MSc, Assistant Professor of Neurology at Rutgers Robert Wood Johnson Medical School and a neuroendovascular surgeon at RWJUH.
Following the successful mechanical thrombectomy, David was moved to the Neurocritical Care Unit, where he was monitored by a specially trained team of neuro-ICU specialists, ICU advanced practitioners and neuro-trained nurses. “He did wonderfully well,” says Dr. Mehta. “His treatment was able to reverse the stroke.”
After a mechanical thrombectomy, most stroke patients require rehabilitation. David was evaluated by physical and occupational therapists at RWJUH, but he didn’t need any services.
“Miraculously, I regained all movement and speech,” says David, who was released a few days later. David had “an amazing recovery because we treated him so quickly after his symptoms began,” says Dr. Mehta.
Today, David takes an aspirin daily. He hasn’t suffered any lasting effects from the stroke.
“The care at RWJUH was amazing,” he says.
The Most Advanced Neurological Care
Robert Wood Johnson University Hospital (RWJUH) was one of the first hospitals in New Jersey to be certified as a Comprehensive Stroke Center. At RWJUH, stroke patients have neurosurgery and subspecialty care in the state-of-the-art Neurocritical Care Unit. “The unit took several years to design and is cutting-edge and patient-focused,” says Kiwon Lee, MD, FACP, FAHA, FCCM, Chief of the Neurology Service and Director of the Comprehensive Stroke Center at RWJUH and Professor of Neurology and Neurosurgery at Rutgers Robert Wood Johnson Medical School.
Recognition
Robert Wood Johnson University Hospital has received several accolades from the American Heart Association/American Stroke Association (AHA/ASA):
- Get With the Guidelines Gold Plus Achievement Award
The hospital has achieved 85 percent or higher compliance with AHA’s standards for stroke care for two consecutive years. - Target: Stroke Honor Roll-Elite Plus
The hospital gives 75 percent or more of ischemic stroke patients intravenous tPA, a clot-busting drug, in one hour or less. More than half of ischemic stroke patients are treated within 45 minutes. - Target: Stroke Honor Roll Advanced Therapy
More than half of stroke patients are treated with endovascular therapy (such as the removal of a blood clot) within 90 minutes. More than half of patients who are transferred from another hospital are treated within an hour.
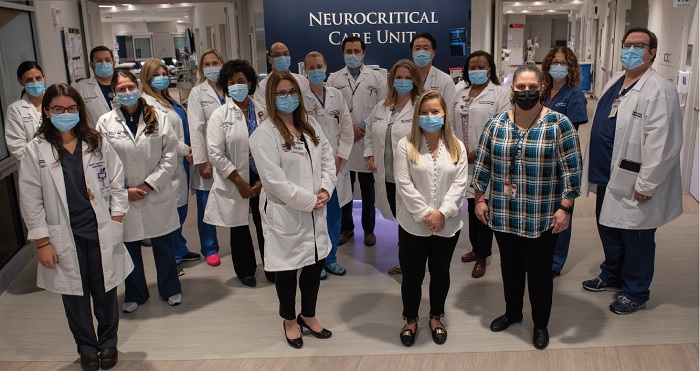
In the Neurocritical Care Unit at Robert Wood Johnson University Hospital, stroke patients are cared for by a multidisciplinary team, which consists of neurologists, neurosurgeons, interventional radiologists and nurses trained to provide neurointensive care.
Signs of a Stroke
With a stroke, “time is brain,” meaning brain cells are lost quickly as a stroke progresses.
Watch for any of the following symptoms, which are represented in the “BE-FAST” acronym:
- B is for balance (trouble walking or loss of balance)
- E is for eyes (trouble seeing)
- F is for face (drooping or numbness)
- A is for arms (weakness or numbness)
- S is for slurred speech or trouble talking
- T time is brain. Call 911 as soon as possible.
*Name has been changed to protect privacy.
Learn more about stroke care at Robert Wood Johnson University Hospital.
