“The nurses were so patient. When you’re dealing with people who are as sick as I was, it takes a special kind of person.”

Kevin Lott, 54, of Clark, is the first to admit that he has never been good about going to the doctor, but his illness in April felt different.
“I hadn’t been well for a couple of months,” recalls Kevin, who works part-time at a hotdog stand. “I smoked at the time, so I already had a cough, but at that point I couldn’t stop coughing. I was having trouble breathing, and it was hard for me to sleep at night.”
In the end, Kevin’s son finally stepped in and convinced his father that he had to go to the hospital.
A Critical Case
It took a village to save Kevin Lott’s life, and the process started with the skilled medical professionals in the Emergency Department (ED) at Robert Wood Johnson University Hospital (RWJUH) Rahway.
“By the time I got there, I was really feeling terrible,” Kevin remembers. “I had a temperature, but I was freezing cold. They brought me warm blankets. One of the nurses said, ‘Close your eyes and relax,’ and that’s the last thing I remember.”
Jordan Greenberg, PA, an emergency medicine physician assistant, oversaw Kevin’s care in the ED.
“Mr. Lott arrived complaining of fever, shortness of breath and body aches,” Greenberg recalls. “He also had an extremely elevated white blood count. The staff and I quickly determined that he had pneumonia.”
In the ED, Kevin was treated with antibiotics as well as oxygen. Because he had no primary care doctor, the on-call physician was contacted, and Kevin was admitted to the Critical Care Unit.
Kevin’s pneumonia triggered a bout of sepsis, a potentially life-threatening complication. Sepsis occurs when the body tries to fight an infection and the immune system goes into overdrive, causing inflammation that can damage organs. Any infection can lead to sepsis, but it most commonly happens with infections of the lungs, such as pneumonia, as well as of the urinary and digestive systems.
Finally Awake
By the time Kevin awoke, weeks had passed. He was still gravely ill, intubated with chest tubes that drained infection from his lungs. He eventually was moved to a regular room in the 3C Unit at RWJUH Rahway, where he remained for an extended period.
“They told me I’d been on a ventilator for a week,” he says. “The doctors kept trying to find new antibiotic combinations that worked.”
He had lost 90 pounds and was so weak that he was unable to lift his legs onto the bed.
“The nurses were so patient,” he remembers. “I had to keep calling them to help me. I pulled out my tubes several times. Everything tasted bad to me, but one nurse’s aide named Nancy kept trying to get me to eat. When you’re dealing with people who are as sick as I was, it takes a special kind of person.”
“When Mr. Lott got here, he was in such a weakened state due to his infections that he required assistance, even with eating. But as time went, on he fought hard to get stronger. It’s great to know that he’s back to himself and that we helped him get there!” says one of his 3C nurses, Jessica Ojibara, BSN, RN.
In mid-May, Kevin finally left the hospital but had to be readmitted a week later because his condition wasn’t stable. He was finally discharged to rehab on June 7.
In September, he visited the hospital wearing a T-shirt with the words “I Believe” and a picture of Santa. “I wanted to see the folks who took care of me and to thank them,” he says.
The medical personnel were thrilled by his visit. “To see him walking around was amazing,” said Nancy Calixte, one of the CNAs who took care of him. “We were so glad. It gave us goosebumps.”
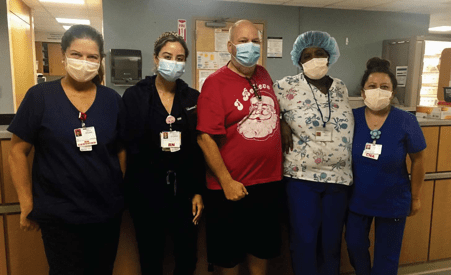
Arlene Turner, RN, Lilliana Alvarado, RN, Kevin Lott, Nancy Calixte, CNA, and Nalda Lynch, CNA.
Listening to Your BodyKevin Lott’s experience highlights the importance of paying attention to your body and addressing symptoms early. In some cases, a change in how you feel physically can alert you to a health problem that can be solved with medication or another minor intervention. Alternatively, it could involve early detection of a more serious illness and prevent a more severe stage from developing. Signs You Should Go to the Doctor
Signs You Should Go to the ED
|
To find a doctor at RWJUH Rahway, call 888-724-7123.