"A lot of men suffer with the problem and don't say anything. I don't want men to neglect their health."
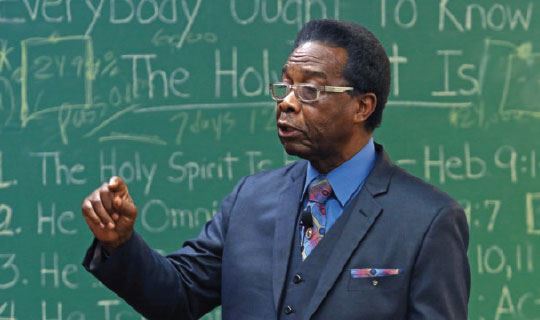
In 2017, Thomas Simpson noticed he was having problems urinating. He had to get up to use the bathroom several times during the night, and at times, he felt like his bladder didn’t empty completely. Occasionally, he also experienced an urgent need to “go.” During the day, he’d have to look for bathrooms just in case he needed them. “I was working a lot and staying up late,” recalls the 72-year-old pastor from Lakewood, who would get up at 5 a.m. and work through the afternoon. “I thought I was under too much stress and wasn’t drinking enough water.” Still, the problems came and went, so Thomas didn’t think there was an urgent need to see a physician.
Then, one day in December 2018, he came home from work and felt ill. He ate a salad with his wife, Janie, and later vomited. She took him to Monmouth Medical Center Southern Campus (MMCSC), where his daughter, Debbie, works as a nurse. “I tried to give a urine sample, but nothing came out,” he recalls. It turns out he had benign prostatic hyperplasia (BPH), or an enlarged prostate gland. (See “What is Benign Prostatic Hyperplasia?”) “Thomas’ gland was severely enlarged, and it was obstructing his urinary stream,” says Mukaram A. Gazi, MD, FACS, Chairperson of Surgery and Chief of Urology at MMCSC.
Clearing the blockage
A tube was placed in Thomas’ bladder to drain the urine. Next, Dr. Gazi performed a cystoscopy, in which a thin, lighted scope is inserted into the urethra—the channel that carries urine out from the bladder—to evaluate the blockage. As Dr. Gazi originally believed, the prostate gland was obstructing Thomas’ urethra, preventing urination. “We needed to open the urethra and preserve bladder function,” says Dr. Gazi.
He performed a procedure known as TURis (transurethral resection in saline), in which the prostate tissue is removed and vaporized in a saline solution. The procedure takes less time to perform and leads to a quicker recovery and fewer complications (less than .1 percent, says Dr. Gazi) than the traditional method.
With the usual method, the prostate tissue is removed in sterile water. This can lead to complications known as post-TURP syndrome, in which the body absorbs fluid from the procedure. This can cause an electrolyte abnormality, as well as an increased risk of bleeding and infection.
A Complete Recovery
 The TURis procedure, which can also be done on an outpatient basis, went smoothly. “Thomas has done phenomenally well,” says Dr. Gazi. “He had no complications.” Thomas was given pain medication after the surgery, but he wasn’t uncomfortable. “I didn’t have any pain, and my appetite was good,” he says. “I had top-of-the-line treatment by all of the nurses around the clock. Dr. Gazi treated me like a family member. This was one hospital stay I enjoyed.” Since the procedure, Thomas has had no trouble urinating. “I’m so glad I had the surgery,” he says. “I feel 100 percent better. Now I have to make myself go to the bathroom. I can also go to bed at 8 p.m. and get up at 4 or 5 a.m. without using the bathroom.” He wants to encourage other men to see their physician or urologist if they’re having trouble urinating. “A lot of men suffer with this problem and don’t say anything,” he says. “I don’t want men to neglect their health.”
The TURis procedure, which can also be done on an outpatient basis, went smoothly. “Thomas has done phenomenally well,” says Dr. Gazi. “He had no complications.” Thomas was given pain medication after the surgery, but he wasn’t uncomfortable. “I didn’t have any pain, and my appetite was good,” he says. “I had top-of-the-line treatment by all of the nurses around the clock. Dr. Gazi treated me like a family member. This was one hospital stay I enjoyed.” Since the procedure, Thomas has had no trouble urinating. “I’m so glad I had the surgery,” he says. “I feel 100 percent better. Now I have to make myself go to the bathroom. I can also go to bed at 8 p.m. and get up at 4 or 5 a.m. without using the bathroom.” He wants to encourage other men to see their physician or urologist if they’re having trouble urinating. “A lot of men suffer with this problem and don’t say anything,” he says. “I don’t want men to neglect their health.”
What is benign prostatic hyperplasia?
The prostate is a small, walnut-shaped gland that creates fluid for semen. It surrounds the urethra, the channel that carries urine out from the bladder. Benign prostatic hyperplasia (BPH) typically occurs with aging (about half of men between 51 and 60 have the condition, and up to 90 percent of men over age 80 have it). When the gland enlarges, it can press on the urethra, irritating or blocking the tube. It can also cause bladder damage and infection. Symptoms include the following:
- A sensation that the bladder is full, even after urinating
- The need to urinate often (every one to two hours)
- An urgent need to urinate
- Weak urine flow
- Trouble urinating (the need to push or strain or stop and start urinating)
To find a urologist at MMCSC, click here or call: 888.724.7123