
 Renuka Verma, MD
Renuka Verma, MD
Section Chief, Pediatric Infectious Diseases,
Unterberg Children’s Hospital at Monmouth Medical Center
Influenza season is upon us and it has shown its ugly head in the pediatric population with significant impact already. Children consistently have the highest attack rates of influenza in the community during seasonal influenza epidemics. They play a pivotal role in the transmission of influenza virus to their households and close contacts (eg, grandparents). Children <5 years (especially < 2 years) and children with certain underlying medical conditions are at increased risk of hospitalization and complications from influenza.
As per CDC, the hospitalization rate in children 0-4 yrs. age group is 9.3/100,000 population, with five deaths reported so far. Of all the specimens tested for respiratory illnesses, 12.8 % are positive for influenza, with 99% being influenza A (H3N2). Hospitals in the lower half of the country are currently faced with significant surge in pediatric hospitalizations and posing challenges for the resources and workforce.
Influenza is a viral infection of respiratory system with systemic symptoms, which may appear to be similar to common cold, however more severe. Signs or symptoms in influenza include sudden fever, headache, body aches, chills, sore throat, stuffy, runny nose, dry cough. Patient can also have fatigue, abdominal pain, nausea and vomiting, diarrhea and conjunctivitis.
Acute influenza can lead to complications such as, pneumonia, invasive bacterial infections (Methicillin Resistant Staph Aureus, MRSA), myocarditis, encephalopathy, Guillain Barré syndrome, sepsis-like syndrome in neonates, exacerbation of asthma or heart disease, Reye syndrome if combined with aspirin, and death. Healthy children are more likely to have complications from influenza, than from COVID-19 infection.
Young children (<5yrs.), Black, Hispanic, American Indian/Alaska Native, and Asian/Pacific Islander people compared with White are at higher risk of severe illness from the fl u.
Treatment
Although best results are observed when patient is treated
with antivirals within 48 hours of symptom onset, however,
therapy should still be considered beyond 48 hours in,
- Any child hospitalized with suspected or confirmed influenza disease.
- Any child with severe, complicated, or progressive influenza disease,
- Any child with suspected or confirmed influenza disease of any severity, and at high risk for influenza complications, regardless of health care setting
Antivirals for Influenza
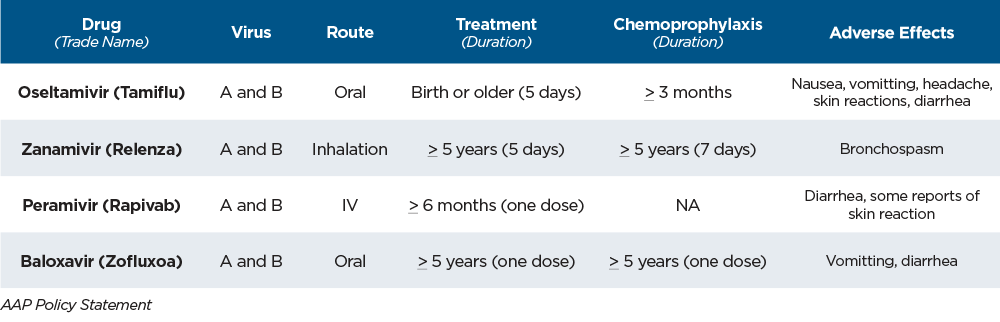
Antiviral chemoprophylaxis is recommended after known or suspected influenza exposure in certain situations, including
unvaccinated staff and children in a closed institutional/household setting with children at high risk for influenza complications
(eg, extended-care facilities), to control influenza outbreaks.
Prevention
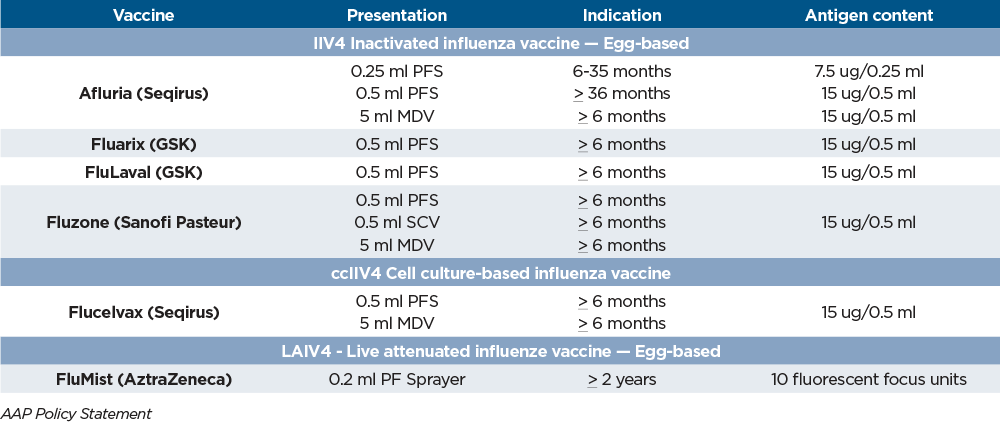
An annual flu vaccine is the best way to protect against flu. CDC recommends that everyone age 6 months and older get a flu vaccine annually. Children 6 months through 8 years of age who are receiving influenza vaccine for the first time, Or only 1 dose ever before July 1, 2022, Or vaccination status is unknown, should receive 2 doses of vaccine 4 weeks apart, ideally by the end of October.
Egg allergy does not increase risk of anaphylactic reaction to vaccination with inactivated influenza vaccines. Children with egg allergies can receive age-appropriate, licensed, recommended vaccine without special precautions beyond those recommended for other routine vaccines. Children with a history of allergic reaction to previous influenza vaccination, should be evaluated by an allergist and vaccine administration should be supervised by a health care provider who can recognize and manage allergic conditions.
Pediatric Vaccines 2022-2023
The ASP, representing pediatric providers, including pediatric infectious disease specialists and pharmacists, exchange ideas, discuss case management strategies and develop and implement guidelines to be shared system wide, as well as serve as a resource for community physicians.
For more educational information, research and best practices from the Children’s Health Network at RWJBarnabas Health, visit rwjbh.org/childrenshealthresearch.