A new study from Saint Barnabas Medical Center shows an increased quality of care provided to patients undergoing cesarean birth. Led by the Clinical Excellence and Effectiveness team at Saint Barnabas Medical Center, these findings, published in Obstetrics and Gynecology – popularly known as "The Green Journal" – was a multidisciplinary effort to create an “enhanced recovery after surgery” pathway for all cesarean deliveries at the medical center.
Enhanced recovery after surgery (ERAS) has become a widely adopted model to increase the quality of patient care through enhanced management of surgical patients in the perioperative period. “ERAS pathways have been adopted in a variety of surgical settings, including colorectal, bariatric, gynecological, hip and knee replacement, and most recently cesarean delivery,” says Paul C. Yodice, MD, FCCP, FCCM, Chair of Department of Medicine and Director of Clinical Excellence and Effectiveness, SBMC. “These pathways have been shown to significantly reduce the length of stay, costs, and in-hospital mortality while increasing the quality of patient care.”
“While the benefits of ERAS programs have been shown, up to this point, little research has highlighted their effectiveness in the cesarean delivery population or shown their effectiveness in reducing opioid usage,” says Richard C. Miller, MD, FACOG, Chair of Department of Obstetrics and Gynecology, SBMC. “The adoption of an ERAS program focused on the cesarean delivery population represents an important opportunity to significantly improve patient care.”
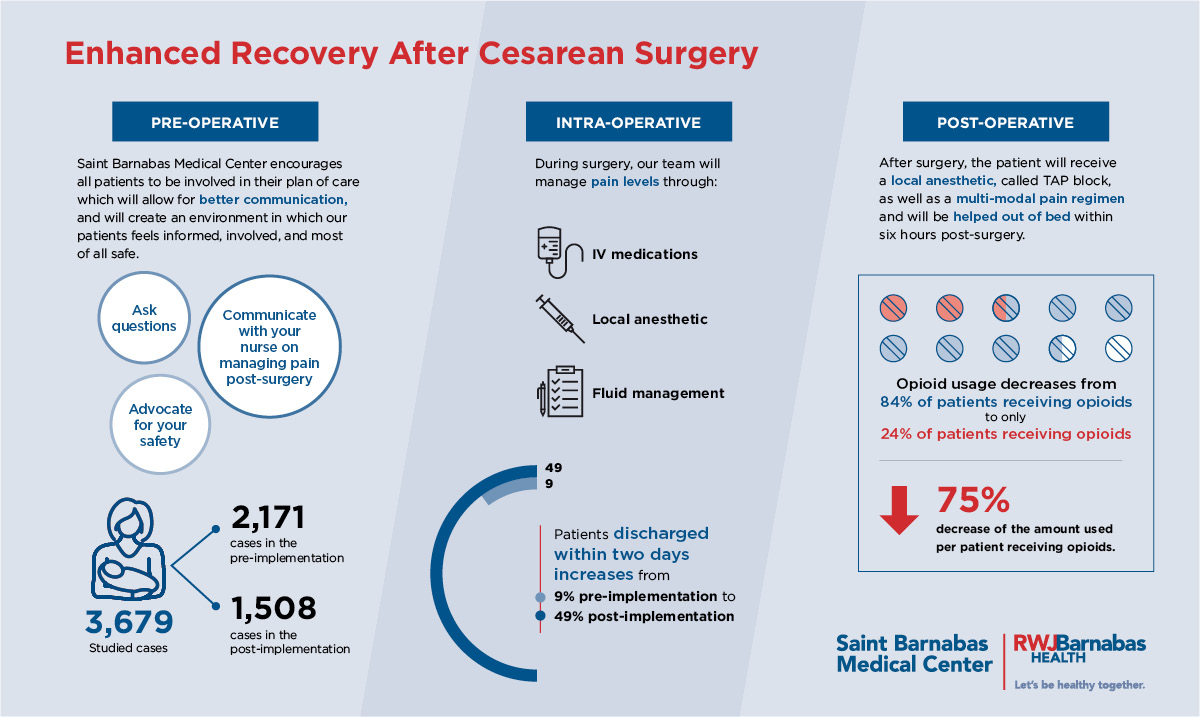
Saint Barnabas Medical Center conducted a study including a total of 3,679 cases, with 2,171 cases in the pre- and 1,508 in the post- implementation periods. “We hypothesized that an ERAS-based approach to the management of cesarean deliveries would have a positive impact on patient outcomes, including decreased length of stay and decreased opioid usage,” says Luciana C. Mullman, MPH, CSSGB, Administrative Director of Clinical Excellence and Effectiveness, SBMC.
As a result, the length of stay, from completion of the cesarean to discharge, decreased significantly post-implementation from an average length of stay of 3.2 days to 2.7 days post-implementation. Furthermore, the percentage of patients discharged within two days improved from 9% pre- implementation to 49% post-implementation.
Additionally, opioid usage decreased significantly in the post ERAS implementation period. Before ERAS pathway implementation, 84% of patients received opioids, while post ERAS implementation, only 24% of patients received opioids. For patients receiving opioids, the amount used per patient is reduced by 75%.
“With the opioid epidemic, it has become increasingly difficult to balance overuse while adequately managing post-operative pain,” says Richard Pitera, MD, Associate Chair of Anesthesia, SBMC. “Through the ERAS program, we identified a procedure, known as TAP [transverse abdominis plane] block, where we can inject local anesthetics into the abdominal wall during surgery as a first step in controlling pain in that area. The TAP block combined with familiar medicines like Motrin and Tylenol, can decrease the patient’s pain by up to 70 percent without the use of opioids.”
Adopting an ERAS approach to cesarean surgery means that more patients are going home faster, in less pain and without a prescription for opioids. Saint Barnabas Medical Center’s efforts are an important step towards ending the opioid crisis in the United States.