By: Musola Oniyide, DPT, Barnabas Health Ambulatory Care Center
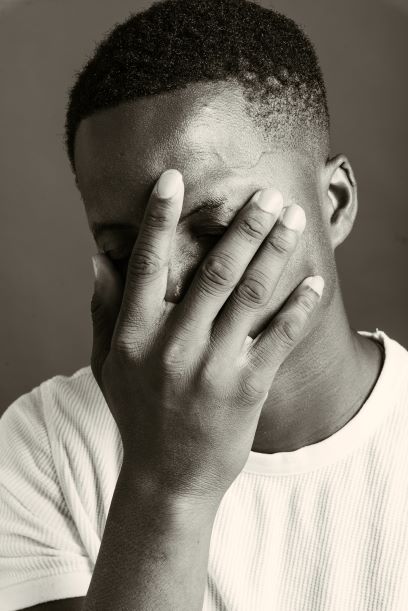
One of the primary reasons individuals seek physical therapy is to eliminate their pain. Pain can be a limiting factor in a person’s ability to participate in essential life activities. These include and are not limited to work, recreational exercise, sports, sleep, and the list goes on. As physical therapists, it is our goal to assist our patients in either eliminating or managing their pain. During the rehabilitation process people tend to embrace misconceptions about pain. These misconceptions act as a barrier between a person and their return to those essential life activities. I’ll discuss the 5 most common misconceptions about pain and hopefully provide clarity regarding pain.
1. “If I move and have pain it means that I am damaging something”
Whenever, a person experiences acute or chronic pain there is an understandable apprehension towards movement. One could suspect that movement triggers pain, resulting in damaged tissues. While this may be true in some cases, like incurring a traumatic injury, it is not true in all cases. Initially, pain is a natural response to potential or actual tissue damage.1 This initial response triggers tissue healing. Despite healing being completed over time, pain signals may still be sent to the brain when movement occurs. This is especially apparent in individuals who experience chronic pain. It is helpful to remember that “Hurt does not always equal harm”. Movement is essential for life and should not be completely ceased due to pain.
2. “I am in pain because there's arthritis in my back, knee, hip, or (insert body part here)”
This thinking is most apparent with individuals who have received imaging such as an MRI or an X-ray. For example, they may receive an X-ray of their lumbar spine which indicates osteoarthritis and degenerative disc disease. This leads to people adopting the misconception that what is shown on the image is directly causing their pain. However, studies have shown otherwise. There have been studies in which a given population of individuals receive imaging of their lumbar spine. Generally, the findings show that all these individuals present with some form of osteoarthritis or degenerative changes in that area. What was also found was that some individuals experienced pain while others did not. These findings suggest that pain is not always directly related to the findings of imaging, but may relate to other factors in a person’s life (diet, sleeping habits, activity level, stress, etc).2 Considering this, it is better to understand imaging as a diagnostic tool, amongst many, which is simply a piece to a puzzle.
3. “No pain, no gain”
My colleagues and I hear this from our patients frequently. It is rooted within our society as a mantra to help motivate us through unpleasant situations; especially when it comes to fitness. Within the context of rehabilitation this saying does not always hold true. If one is experiencing muscle soreness following an exercise given by a physical therapist, that is a natural and beneficial response. However, intense pain accompanied by muscle soreness during an exercise will most likely not result in rehab gains. In most cases this is indicative of improper technique of an exercise, too much resistance, or too many repetitions. In rehab, exercise is meant to be therapeutic in addressing a patient's complaint of pain, if an exercise precipitates it needs to be altered.
4. “As long as I have pain I will be completely unable to do what I love or need to do”
Embracing this misconception can prevent people from fully returning to their activity of interest. This could possibly be out of the fear damaging tissue (which I address above) or re-injuring one’s self. As I discussed before the onset of pain during activities, especially later in the rehab phase, is not indicative of tissue damage. Considering this, one can participate in their activities of interest as long as their pain does not rise to a significant intensity. This may mean that some individuals may have pain with functional activities, but at a lower intensity after completing their rehabilitation. What is of priority is being able to participate in the function of interest with minimal pain at the least.
5. “Medications such as pain killers are the only way to address my pain.”
When individuals experience pain, acute or chronic, medications are usually prescribed by their referring physician. On occasion people may have the misconception that the medication is addressing the root issue. While pain medications do reduce one’s perception of pain, the effect is temporary. People forget or are unaware that the main culprit of their pain is usually a musculoskeletal issue. This is best addressed with therapeutic exercise and manual therapy provided by a licensed physical therapist. Additionally, research has shown that exercise and aerobic activity play an effective role in reducing one’s perception of pain.3 To adequately address one’s pain there needs to be an accurate understanding of the cause of their pain.
In summation, these are 5 misconceptions I sought to shed light upon. By having a clear and research based view of pain, people are able to address it with viable methods. One should note that in post-surgical cases these “rules” may be different due to the time needed for bone and soft tissues to heal. Additionally, it is important to consult a licensed physical therapist regarding issues with pain associated with activities of interest. By disregarding these misconceptions one’s rehabilitation process can be more fruitful allowing them to return to their activity of interest at an optimal level.
References
- Khalid, Shehzad, and R. Shane Tubbs. "Neuroanatomy and neuropsychology of pain." Cureus 9.10 (2017).
- Rahyussalim, Ahmad Jabir, Muhammad Luqman Labib Zufar, and Tri Kurniawati. "Significance of the association between disc degeneration changes on imaging and low back pain: a review article." Asian spine journal 14.2 (2020): 245.
- Gordon, R.; Bloxham, S. A Systematic Review of the Effects of Exercise and Physical Activity on Non-Specific Chronic Low Back Pain. Healthcare 2016, 4, 22.
Musola’s Bio:
Musola Oniyide is a physical therapist at the Barnabas Health Ambulatory Care Center in Livingston with a focused interest in the study of pain science. His primary goal with his patients is to optimize their function so that they can live their best lives. Whenever he is not doing that he is drawing, completing home workout programs, reading graphic novels, playing video games, reading books related to religion & philosophy, or traveling the world.
The Saint Barnabas Medical Center Rehabilitation centers are open and ready to help you achieve your goals. With four locations in West Orange, Millburn and Livingston, the experienced and compassionate staff at Saint Barnabas Rehabilitation offers adults and children the specialized care they need to resume an active life after surgery, injury or illness. They are committed to providing patients with the most advanced services in a safe, caring and soothing environment. For high-risk patients who are unable to visit in person, telehealth is an option. Patients do not need a prescription for physical therapy services.