“When I am not managing the ride, I am thinking about managing the ride,” said Gerald. “It is important to be able to work while I wait for my transplant.”
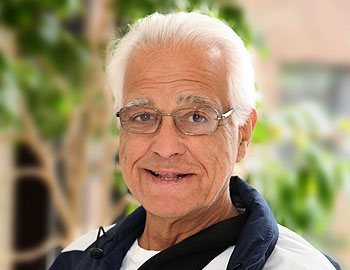
Gerald, 66 of Staten Island, has been passionate about running the Cyclone rollercoaster at Coney Island for 35 years. With the world’s most advanced ventricular assist device (VAD) replacing the pumping action of his heart, he will be at his post again this year when the amusement park opens on Sunday, March 28.
“When I am not managing the ride, I am thinking about managing the ride,” said Gerald. “It is important to be able to work while I wait for my transplant.”
Diagnosed with end-stage heart failure, Gerald’s heart stopped in December 2009 at a family birthday party. His health declined quickly and his wife and daughters thought it was the end until doctors at the Heart Failure Treatment and Transplant Program at Newark Beth Israel Medical Center implanted a revolutionary VAD to support Gerald’s heart while he waits for the heart transplant he needs.
The VAD known as the DuraHeart is the most technologically advanced heart pump currently in clinical study in the United States. The Heart Center at Newark Beth Israel Medical Center is only the fourth program in the country to implant it and the only center in New Jersey offering this extraordinary treatment for end-stage heart failure.
Gerald has never ridden the coaster, but it is not because he is afraid of heights. “It’s the drop I don’t like,” he said. Over the years he walked every inch of the track many times. Born and raised in the shadow of the world’s most famous rollercoaster, Gerald was hired in 1975 to help renovate of the old ride and hasn’t missed an opening day since. Today, he is Manager of the Cyclone and still enjoys watching young and old enjoy the thrill.
Gerald is among more than 6,000 people who have received VADs in the United States. Newark Beth Israel Medical Center is one of the nation’s most experienced and active implant centers. Since they implanted NJ’s first VAD in 1993, cardiologists and cardiac surgeons at the Heart Center at Newark Beth Israel continue to advance research in the field and broaden use of the devices. Experts from other heart centers in the region come to Newark Beth Israel to receive training and gain competence in the use of a variety of VADs.
“Once reserved as a treatment of last resort for people with end-stage heart failure, the latest generation of pumps is enhancing the quality of life for people with less severe heart failure,” explained Mark J. Zucker, MD, JD, Director of Heart Failure Treatment and Transplant at the Heart Center at Newark Beth Israel Medical Center who has been involved with the application of mechanical assist devices since the 1980s. “Potentially, more than 40,000 Americans will need a heart transplant and only about 2,500 donor hearts are available each year. We are compelled to explore alternative treatments for advanced heart failure.”
Gerald’s small, silent DuraHeart is a stark contrast to the first clunky heart pumps that whirred and ticked and rarely lasted for more than several months. Weighing nearly four pounds, the early devices were so big that they were only suitable for patients with a large frame, which excluded most women from this treatment option. Furthermore, their complex function and maintenance often kept patients hospitalized for as long as the pump remained implanted.
The DuraHeart represents several leaps forward in heart pump technology. For example, the two moving parts that comprise the three-inch-diameter pump are separated by electromagnetic levitation that eliminates mechanical friction and prevents damage to delicate blood cells as they flow through the pump. The DuraHeart even has the capability to speed up or slow down in response to the body’s changing activity level and the native heart’s ability to carry the load.
The newest VADs can be a bridge to transplant or provide therapy for people who are not eligible for a transplant. “Mechanical circulatory assist devices have advanced so dramatically in the last two decades that the field of cardiology is seeing a rapid expansion of this therapy,” said Margarita Camacho, MD, Surgical Director of Cardiac Transplant and Assist Devices, Heart Center at Newark Beth Israel Medical Center. Dr. Camacho chairs the Society of Thoracic Surgeons national Workforce on the Surgical Treatment of End Stage Cardiopulmonary Disease and is spearheading simulated computer VAD training. “Today’s VADs have the potential to function for up to three to five years and perhaps longer while people resume active lives at home,” she noted.
Unlike other centers that provide limited VAD implantation, Newark Beth Israel’s comprehensive VAD services are completely integrated with its heart transplant program, ensuring that each patient is thoroughly and continually evaluated or all treatment options. Newark Beth Israel’s heart transplant program ranks among nation’s top ten by volume and has consistently achieved short- and long-term graft survival rates that meet or match national benchmarks.