Program Details
Educational Goals and Objectives for the Thoracic Surgery Fellowship Program
The overall goal of the Thoracic Surgery Fellowship is to graduate physicians proficient in providing safe, cost effective, timely, patient centered, high quality care in the following areas: Pre-operative, operative, post-operative including critical care of the patients with pathologic conditions within the chest. This includes surgical care of diseases of heart (coronary artery disease, valvular heart disease) and great vessels, lungs, airways, esophagus, chest wall, mediastinum, diaphragm and chest injuries. The necessary emphasis is also given to congenital cardiac surgery, cardiothoracic transplantation and mechanical circulatory assistance.
The fellows selected into our program will have completed an accredited General Surgery Residency Program. This individual will have the necessary skills and knowledge in surgical principles, techniques, and management of disease processes. The focus of our program is to build on these strengths and accomplishments. He/she will be given graduated responsibilities with supervision to diagnose and treat thoracic illnesses, both surgically and non-surgically as indicated, in a patient centered environment. The clinical learning environment is conducive to delivering safe, effective, cost efficient, timely, compassionate care while preserving the patient confidentiality.
The educational goals and objectives we aim to achieve —
The fellow will:
- Have intense training in the necessary basic sciences to understand and manage thoracic diseases in general and cardiac diseases in particular.
- Gain competence in in the following: diagnosis, comprehensive treatment plan, counselling and advocating the patient/family regarding the disease, treatment options, prognosis with and without the proposed treatment, risks, benefits and alternatives to the planned therapy and details of the procedure being proposed.
- Be adept in preoperative preparation, conduct of safe, efficient, and effective surgery and post-operative care.
- Have the ability to utilize resources and tailor the best treatment for the patient in the current and evolving health care environment (systems-based practice).
- Understand his/her own abilities, limitations, and seek help in the best interest of the patient and refer the patient to a physician/place of excellence when appropriate.
- Function effectively and collegially in the health care environment.
- Maintain a culture of life long education and scholarly activities to remain proficient in the knowledge of established and evolving biomedical, clinical, epidemiological, and social behavioral sciences and well as the application of this knowledge to patient care.
- Incorporate practice-based learning and continuously improve patient care.
- Learn the methods and participate in quality improvement to implement appropriate changes in patient care throughout their career.
- Learn to be compassionate towards the patients and families, respectful of other professionals and colleagues, respect privacy, and maintain integrity and accountability.
- Participate in local, regional, and national organizations in thoracic surgery.
In order to achieve the stated goals the program will:
- Maintain regular didactic and clinical educational sessions.
- Provide necessary tools both electronic and otherwise.
- Provide assignments at each educational level.
- Clearly delineate responsibilities in patient care and progress responsibility as appropriate.
- Provide sufficient and constant faculty supervision throughout the program.
- Cover all the topics and competencies in the curriculum as recommended by the ACGME/TSDA/STS.
- Assist in accomplishing all procedural skills necessary to become an independent, proficient Cardiothoracic Surgeon.
- Provide regular faculty member and program director’s evaluation and recommendations.
- Organize a clinical competency committee and program evaluation committee to assess, evaluate, and take steps to improve any deficiencies on an ongoing basis.
- Provide the fellow with the opportunity to evaluate program periodically and make recommendations.
- Provide the fellow feed- back with the input of the Program Director, faculty members, and 360-degree evaluations on a biannual basis at minimum.
- Provide clear guidelines for the trainee to follow.
The program will maintain didactic and clinical education, in an environment of learning, manage fatigue, provide for work-life balance, while evaluating and counselling on an ongoing basis to facilitate growth towards accomplishment of clinical proficiency and independence.
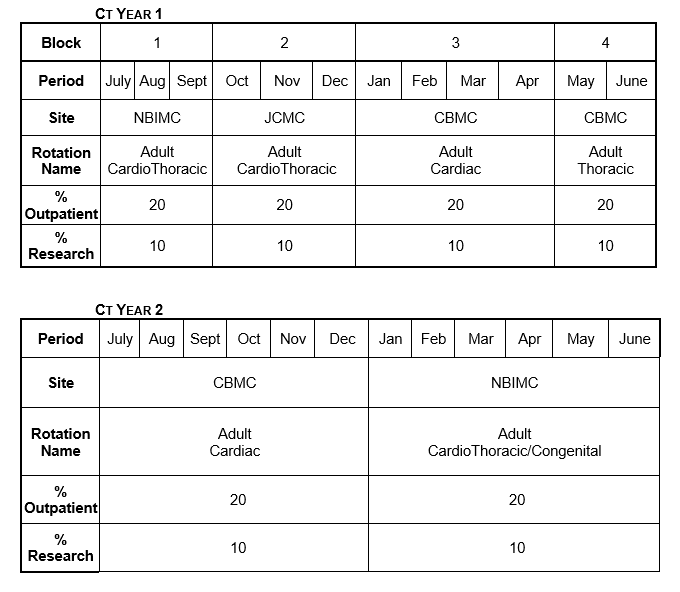
Block Schedule
Site 1 – Newark Beth Israel Medical Center (NBIMC)
Site 2 – Cooperman Barnabas Medical Center (CBMC)
Site 3 – Jersey City Medical Center (JCMC)
Adult cardiothoracic and congenital cardiac training will take place at Newark Beth Israel Medical Center concurrently. Fellows will also participate in General Thoracic Surgery cases at this site when possible, especially emergencies and complex cases to gain additional experience without encroaching on the training of General Surgery Residents. Residents are required to attend structural heart courses and assist in these cases throughout the fellowship. The fellows are encouraged to get involved in Heart failure, Heart transplantation, Mechanical circulatory assistance, and lung transplantation whenever there is opportunity throughout their fellowship.
The Jersey City Medical Center is an elective rotation in Adult Cardiothoracic Surgery during the months of October, November, and December.
The emphasis during the first three months (July, August, and September) of rotation at Newark Beth Israel Medical Center is to gain experience in preoperative, post-operative, critical care of the cardiac surgical patient and gain basic operative experience. During this three months rotation, the resident has to complete all required courses for the hospital, system, and graduate medical education. During the next four months, (January through April) the resident will rotate in cardiac surgery service at Cooperman Barnabas Medical Center . This rotation will provide the resident exposure to all aspects of adult cardiac surgery. It is an exclusive rotation in cardiac surgery and the resident will be involved in all aspects (I.E.), pre, intra, and postoperative care, of adult cardiac surgical patients.
The next two months (May and June) rotation is at Cooperman Barnabas Medical Center , in adult Thoracic surgery service. This is an exclusive Thoracic Surgery Rotation and the resident will be involved in all aspects of thoracic surgical practice under the supervision of the Director of Thoracic Surgery, Dr. Joanna Sesti.
Congenital Cardiac Surgery
The congenital cardiac surgery at Newark Beth Israel Medical Center / Children’s’ Hospital of New Jersey, is active and growing. In order to gain maximum exposure, the senior fellow will avail himself to the extent possible, to participate in that service. The senior year is spent at Newark Beth Israel Medical Center learning adult and congenital cardiac surgery.
Outpatient
During all rotations, fellows will spend twenty percent of their time in outpatient clinic. They will have (on average) one day per week dedicated to managing pre and postoperative patients during the office hours.
The model that will be in effect is one where, for combined Cardiothoracic Service in Newark Beth Israel Medical Center and Cooperman Barnabas Medical Center , both the residents will be responsible as a team, with regular rounds, participation in surgery, postoperative care, outpatient practice, under close supervision by faculty, with proper hand off between the two fellows and other involved health care providers. This allows maximum exposure of clinical, research, educational material to both fellows. The close proximity of both institutions lends itself to such a structure.
Research
Fellows will participate in research during all rotations. This is not a structured research time. The program director, faculty member, and chair will assign the research projects. Fellows will work on research during their off-duty time.
Vacation
Fellows will have a total of four weeks of vacation per year. The vacation will only be allowed in one week duration at a time. Only 1 week can be taken during the Jersey City Medical Center rotation and no vacation is allowed during the Thoracic rotation (months of May and June of the first year). Fellows are not allowed to be on vacation at the same time. Holidays are determined by the hospital. Coverage for the holiday is decided with mutual consultation between the fellows with only 1 fellow taking off. The number of holiday coverage will be equally split between the 2 fellows. No vacation time is allowed in the fellow’s terminal month.
Conference Schedule
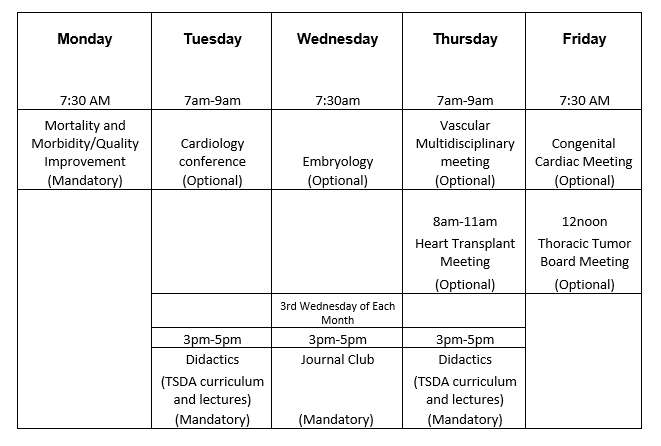
The Journal Club is third Wednesday of every month in the evenings in G5 conference room with occasional exceptions of off-site meetings.
Grand Rounds are in September, December, March, and June. The Grand rounds occur on Third Wednesday morning between 7:30am and 8:15am.
June Grand Rounds speaker will be the graduating chief fellow.
All meetings are either virtual or hybrid virtual / in person depending on the environment.
If the didactics are truncated or cancelled, every attempt is made to conduct them during similar timings of other week-days.
