What to Expect After Spine Surgery
Spine Precautions
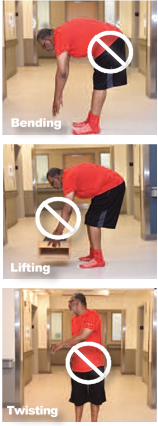
After surgery, you will slowly increase what you do each day. It is also important to plan time to rest. This will help you recover. You will also need to follow spine precautions.
You can use the pneumonic BLT:
- B: No Bending.
- L: No Lifting.
- T: No Twisting, pulling, pushing, or reaching.
- Do not pick up anything heavier than 5 pounds (unless instructed by surgeon).
- Women’s purses can weigh more than 5 pounds.
- A package of sugar weighs 5 pounds.
- A gallon of milk can weigh 9 pounds.
- Do not pick up young children.
Discharge
 You must arrange for an adult driver to take you home after your surgery.
No patients who receive anesthesia can drive, or take county transportation
or taxi service home. Taxi service is only acceptable if you are accompanied
by an adult (over 18 years of age).
You must arrange for an adult driver to take you home after your surgery.
No patients who receive anesthesia can drive, or take county transportation
or taxi service home. Taxi service is only acceptable if you are accompanied
by an adult (over 18 years of age).
It is important for you to make plans before surgery for care at home. Many patients should expect to go directly home. Understanding your plan for discharge is important in the recovery process. You can expect help from the team to develop a plan that meets your particular needs. Many patients should expect to be able to go directly home, as is usually best to heal in the privacy and comfort of your own home.
A patient’s stay in a rehab facility must be done following the guidelines established by Medicare or other insurers.
You will either meet the criteria to go to a rehab facility or your insurance company may recommend that you return home with other care arrangements.
Also keep in mind that insurance companies do not get involved in social issues, such as lack of caregiver, animals, etc. These are issues you will have to address before admission. Again, it is important for you to make plans before surgery for care at home after surgery.
Pain Management
After surgery you will most likely be in pain. Our goal is to manage your pain, not get rid of your pain completely. Pain can be chronic (lasting a long time) or intense (breakthrough). Pain can change through the healing process.
Using a pain scale to describe your pain will help the team understand your pain level. If “0” means you have no pain and “10” means you are in the worst pain imaginable, how would you rate your pain? With good communication about your pain, the team can make changes to make you more comfortable. Try to relax, when you are relaxed medication works better.
Pain can come from multiple nerve pathways in your body. To help manage your pain after surgery your surgeon may use pain control called multimodal analgesia.
Multimodal analgesia means that you will get two or more medications that lessen pain and when used together, they can block more pain signals. Multimodal analgesia is focused on lowering your pain after surgery to help you heal more quickly and easily.
One of the biggest goals of multimodal analgesia is to lessen your need for opioid medications or narcotics. Opioid medications include drugs that come from the opium plant (such as morphine) and also man-made drugs designed to have similar pain reducing effects (oxycodone and hydrocodone).
Opioid medications provide pain relief, but taking them regularly can lead to physical dependence and, sometimes, addiction. Using less opioid medication can help lower the chance of dangerous side effects and also other side effects (such as sleepiness, nausea, vomiting and constipation) that may be unpleasant for you and may disturb your ability to participate in physical therapy.
Multimodal analgesia includes medications that you take before, during, and after surgery. Some of these medications may be familiar to you; for example, acetaminophen (Tylenol). Opioid medications are also used, especially when other medications do not give you enough pain relief.
What Can I Do to Lessen the Pain?
There are many ways to lessen pain. Work with your health care team to find the best ways.
-
Ice
- Ice is a good way to lessen pain.
- Ice should be used right after surgery around the incision.
- Ice should NEVER be placed directly on bare skin. Keep ice packs wrapped in a towel or placed over clothing.
- Ice for 20 minutes at a time. Ice should be off at least 20 minutes unless your facility uses Polar Care.
-
Heat
- Heat can also be used to help the motility/movement of your GI tract following surgery.
-
Stay active
- Get up and move around as instructed.
- Change positions to relieve pain.
-
Relax
- Rest. Make sure you are getting enough, good quality sleep.
- Meditation. This can help focus tour mind and let you relax.
- Music. Find music that is calming or enjoyable to you. This can also help with relaxation.
- Breathing exercises. Slow, deep breathing can reduce stress and pain.
Deep Breathing and Coughing
To prevent potential problems such as pneumonia, it is important to understand and practice breathing exercises. Techniques such as deep breathing, coughing, and using an incentive spirometer may also help you recover more quickly.
Deep Breathing Exercises
- Perform in an upright, sitting/leaning forward/standing position, shoulders relaxed.
- Breathe in deep and slow as much as possible through nose or mouth.
- Hold breath for 2 to 5 seconds
- Then breathe air out slowly through pursed lips (like you are blowing out birthday candles) as a normal relaxed expiration.
- 10 to 15 consecutive breathes repeated for 3 sets with a 60-second pause between each set
-
Cough during pause to mobilize secretions if necessary.
**Perform hourly after surgery**
To Help You Cough
- Take a slow deep breath. Breathe in through your nose and concentrate on filling your lungs completely.
- Breathe out through your mouth and concentrate on your chest emptying completely.
- Repeat with another breath in the same way.
- Take another breath, but hold your breath and then cough hard. When you cough, focus on emptying your lungs.
- Repeat all steps twice.
Constipation Management
Constipation can be uncomfortable and may prevent eating a healthy diet. Constipation can be caused by:
- Not drinking enough fluids
- Use of opioids
- Decreased activity or mobility
To help prevent constipation, you should use a combination of things:
- Drink plenty of fluids, up to 8 glasses of water per day (soda, coffee, and alcohol do not count towards your daily water intake).
- Decrease the use of opioid pain medicine.
- Stay active, get up and move as you are able.
- Eat prunes or drink prune juice. These are natural laxatives. Try this before medicines.
If you are still constipated, a stool softener or laxative may help. If you reach a point when you stop passing gas, this may be a medical emergency.
Caring for Yourself at Home
- Gradually wean yourself from prescription medication to a non-prescription pain reliever. Ask your physician for narcotic alternatives.
- Change your position every 45 minutes.
- Try not to nap too much: While you are recovering, try not to nap too much during the day so that you will sleep better at night.
- Body Changes: Your appetite may be poor. Drink plenty of fluids to keep from getting dehydrated. Your desire for solid food will return.
- You may have difficulty sleeping, which is normal. Do not sleep or nap too much during the day.
- Your energy level will be decreased for at least the first month.
- Pain medication that contains narcotics promotes constipation. Use stool softeners or laxatives, if necessary.
What If I Live Alone?
You may return home and receive help from a relative or friend, or plan to stay at their home for the first few days. Some patients are candidates for a home health nurse to visit them at home for a short while. Please discuss this with your case manager after surgery.
Dressing Change Procedure
Each patient is different, and each surgeon has his own preferences, please follow the instructions of your discharge nurse in the hospital. Don’t forget to wash your hands before caring for your wound.
What Can I Do to Prevent Infection?
- Sleep in clean pajamas and wear clean clothes at home. This makes sure fabric that is close to your incision is clean
-
Keep pets off of your bed or chairs and away from your incision
- Pets can carry germs
- Pets like to lick wounds so keep your incision covered when around them
- Be sure to wash your hands after touching pets
Signs of Infection
- Increased swelling and redness at incision site
- Change in color, amount, or odor of drainage
- Increased pain at surgery location
- Fever greater than 101.5 degrees
Signs of Blood Clots in Legs
- Swelling in thigh, calf, or ankle that does not go down with elevation.
-
Pain, heat, and tenderness in calf, back of knee or groin area.
NOTE: blood clots can form in either leg.
To Help Prevent Blood Clots
- Perform ankle pumps
- Walk several times a day
- Take your blood thinners as directed
Pulmonary Embolus
An unrecognized blood clot could break away from the vein and travel to the lungs. This is an emergency and you should CALL 911 if suspected.
Signs of a Pulmonary Embolus
- Sudden Chest Pain
- Difficult and/or rapid breathing
- Shortness of breath
- Sweating
- Confusion
Prevention of Pulmonary Embolus
- Prevent blood clot in legs
- Recognize if a blood clot forms in your leg and call your physician promptly
Postoperative Safety and Avoiding Falls
Kitchen
- Use a mop and long-handled brushes.
- Plan ahead! Gather all your cooking supplies at one time. Then, sit to prepare your meal.
- Place frequently used cooking supplies and utensils where they can be reached without too much bending or stretching. To provide a better working height, use a high stool, or put cushions on your chair when preparing meals.
Avoiding Falls
- Pick up throw rugs and tack down loose carpeting. Cover slippery surfaces with carpets that are firmly anchored to the floor or that have non-skid backs.
- Be aware of all floor hazards such as pets, small objects, or uneven surfaces.
- Provide good lighting throughout your home.
- Install nightlights in the bathrooms, bedrooms, and hallways.
- Keep extension cords and telephone cords out of pathways. Do NOT run wires under rugs, this is a fire hazard.
- Do NOT wear open-toe slippers or shoes without backs. They do not provide adequate support and can lead to slips and falls.
- Sit in chairs with arms. It makes it easier to get up.
- Rise slowly from either a sitting or lying position to avoid getting light-headed.
- Do not lift heavy objects for the first three months and then only with your surgeon’s permission.
Driving
- It will take at least 2 weeks or possibly longer before you are able to drive.
- Please arrange in advance for transportation during this time.
Sitting
- Limit sitting to 30 to 40 minutes at a time.
- Avoid soft sofas, deep chairs, recliners and chairs with wheels.
- Sit in a chair that has back support and armrests.
Bathing
- Use non-slip bathmat on bathroom floor and in shower/tub.
- Sit on a shower seat/chair.
- Use grab bars for balance.
- Do not shower if your drain is in place.
Intimacy After Surgery
- Ask your doctor when it is safe to have sex.
- Ask what precautions you should follow.
- You may need to try new positions. Some positions are more comfortable and safer.
Postoperative Recovery and Rehabilitation
Life After Surgery

- Be patient with recovery.
- May take 3 months to a year to get desired result
- Be positive. A good attitude leads to better and faster recovery.
- Do not stop doing things if you still have pain. Find a less painful way to do it.
- Less activity may cause stiffness and more pain.
Follow Up With Your Surgeon
You will need to follow-up with your surgeon 2 to 4 weeks after your surgery. Please call your surgeon's office and make an appointment if you have not already done so.
Important Things to Know
-
Signs of infection
- Increased swelling and redness at incision site
- Change in color, amount, odor of drainage
- Increased pain in knee
- Fever greater than 101.5 degrees
-
Signs of blood clots in legs
- Swelling in thigh, calf, or ankle that does not go with elevation
-
Pain, heat, and tenderness in calf, back of knee or groin area
NOTE: blood clots can form in either leg.
-
To help prevent blood clots
- Perform ankle pumps.
- Walk several times a day.
- Take your blood thinners as directed.
Pulmonary Embolus
A pulmonary embolus is an unrecognized blood clot that could break away from the vein and travel to the lungs.
This is an emergency and you should CALL 911 if suspected.
Signs of a pulmonary embolus include:
- Sudden chest pain
- Difficult and/or rapid breathing
- Shortness of breath
- Sweating
- Confusion
Patient Experience Survey
From the time of discharge to perhaps a year later, you may be asked to participate in patient satisfaction surveys. These surveys, both from the hospital and from the Spine Surgery Program, are your chance to tell us what you feel went well and what can be better.
